Introduction
The European LeukemiaNet (ELN) 2017 classification for acute myeloid leukemia (AML) stratifies patients in 3 risk categories, according to genetic features of the disease. ELN classification is commonly used to guide post-remission treatment; favorable risk patients do not seem to benefit from allogeneic hematopoietic transplantation (alloHCT) in first complete remission (CR1) while this procedure is highly recommended in adverse risk patients. Post-remission treatment in intermediate risk patient is still debated. This classification has not been prospectively validated. Herein we analyze the prognostic impact of ELN 2017 classification in patients treated with the same protocol (CETLAM-12), including a well-defined preplanned alloSCT policy according to genetic risk.
Methods
We analyzed characteristics and outcome of patients diagnosed with de novo AML, included in CETLAM-12 protocol for patients up to 70 years, with an available genetic characterization at diagnosis allowing an accurate ELN 2017 stratification. Genetic risk allocation was based on cytogenetic analysis and pre-specified RT-PCR of determined markers (including CBF-rearrangement, NPM1, FLT3, CEBPA, and MLL-PTD) performed in all patients, and targeted Next Generation Sequencing testing (available in 143 patients). CETLAM-12 protocol defines a genetic risk stratification in three groups, closely similar to that proposed by the ELN 2017 classification, and recommends a post-remission strategy based on this risk assessment. Patients from the favorable group received three courses of consolidation with high-dose cytarabine (HiDAC), whereas alloSCT in CR1 is strongly recommended for intermediate and adverse risk patients following one HiDAC-based consolidation course.
Results
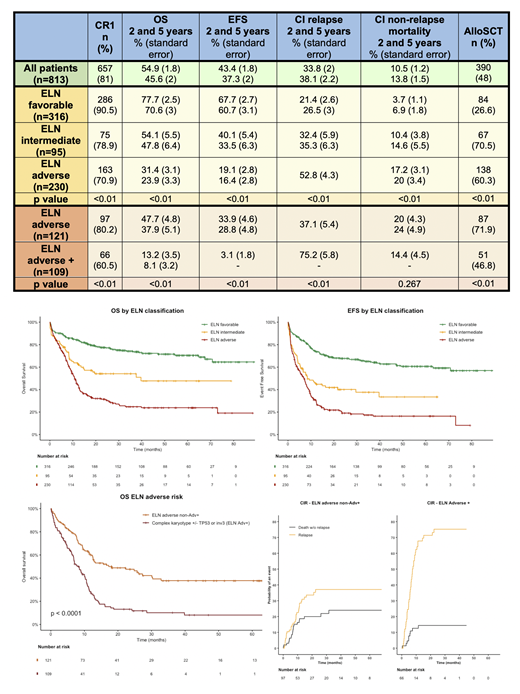
We included in the study 813 patients (400F/413M; median age 56, 17-76); with a 37 months median estimated follow-up (range 0.1-92). The outcomes of the entire cohort are shown in table 1. Out of all patients, 641 could be classified according to the ELN 2017 classification, due to the presence of risk defining genetic features identified by any of described methods.
In the group of .atients allocated in the favorable risk category (n=316; 49%), twenty-seven patients died during induction. Fifty-eight relapses were observed, mostly in patients with NPM1 mutation (n=41). AlloSCT was finally performed in CR1 in 84 patients (27%) due to MRD persistence or reappearance (n=40), overt hematological relapse (n=27), persistent aplasia following chemotherapy (n=3) and protocol deviation (n=14).
In the group of patients allocated in the intermediate risk category (n=95; 15%), twelve patients died during induction. AlloSCT in CR1 was performed in 62 patients (67%), with 5 patients receiving an alloSCT in CR2.
In the group of patients allocated in the adverse risk category (n=230; 36%), twenty-five patients died during induction. AlloSCT could be finally performed in CR1 in 138 patients (60%) and 88 relapses occurred (42 before alloSCT, 46 after alloSCT). Amongst ELN adverse risk patients, a subgroup with a significant worse outcome has been identified, defined by AML with complex karyotype +/- TP53 mutation or chromosome 3q26/MECOM-GATA2 rearrangement. This group (ELNadv+) presented a lower CR rate, with a higher relapse rate and fewer proportion of patients who receive a pre-planned alloSCT in CR1. OS and EFS of ELNadv+ is significantly lower than ELN adverse patients. In the multivariate analysis for OS including age, sex, WBC count at diagnosis and number of cycles to achieve CR, only age and ELNadv+ status showed independent prognostic value.
Outcome data is summarized in table and figures attached.
Conclusions
The initial risk-adapted post-remission assignment planned in CETLAM-12 could be performed in the majority of patients. Despite this different proposed post-remission treatment, ELN risk classification was able to identify three groups of patients with a markedly different outcome. Interestingly, within the unfavorable ELN category, a very high-risk ELNadv+ subgroup can be distinguished, with a dismal outcome with current approach, warranting the implementation of innovative pre and post-transplant strategies aimed to prevent treatment failure.
Tormo:MSD: Honoraria; Janssen: Honoraria; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees; Pfizer: Honoraria; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Daiichi Sankyo: Honoraria; Servier: Honoraria; Roche: Membership on an entity's Board of Directors or advisory committees; Astellas: Membership on an entity's Board of Directors or advisory committees. Salamero:Pfizer: Consultancy; Jazz Pharmaceuticals: Consultancy, Honoraria; Daichii Sankyo: Honoraria; Novartis: Consultancy, Honoraria; Celgene: Consultancy, Honoraria. Sierra:Jazz Pharmaceuticals: Research Funding; Pfizer: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Daiichi Sankyo: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Abbvie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Astellas: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Roche: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Gilead-Kite: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal